Toxic plant pigweed (also known as rough cocklebur, cockleburr), scientifically known as Xanthium strumarium, is a native, annual, invasive plant that grows one to three feed tall. It grows in disturbed areas, sandy soils, and in wet areas like washes and creeks. Leaves can grow large and are triangular in shape. The seed is football shaped with spiny burrs that stick to clothing, animal fur and skin. The seed turns brown when dry. The plant reproduces only by seed.
Affected livestock
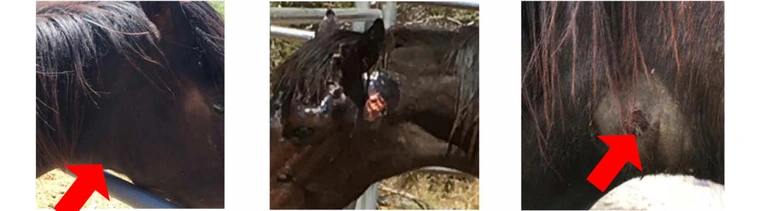
All classes of livestock and poultry are affected by both the seed and the plant. The plant is the most toxic when it is a seedling, but can remain toxic as it grows. Both seeds and young plants contain carboxyactractyloside. Animals can be poisoned by eating less than 0.3% of its body weight of the plant. If not grazed, the plant may be accidentally baled in hay or processed with grain. The seed is covered in many sharp spines that can get stuck in the animals mouth or skin.
Symptoms
Slight to severe hypoglycemia, depression, weight loss, difficult or labored breathing, weakness, convulsions with head and neck spasms, and slow death up to 3 days or sudden death. Clinical signs in goats may mimic polio. Animals who do not die may have liver and gallbladder damage.
Treatment
Remove animals from problem grazing area. Provide shade, fresh water and quality hay that is free from other weeds or toxins. See veterinarian immediately. Prognosis is bad if poisoning is not caught early or quickly.
Prevention
Remove the plant by hand (wear gloves) or use approved herbicide for broadleaved
plants.