Most hantavirus cases in the United States (U.S.) occur in western states and are often concentrated in the Four Corners region of the Southwestern U.S., this specifically refers to the region that connects Arizona, Utah, Colorado, and New Mexico. Hantavirus awareness increased during 2025 due to fatalities reported in California, Arizona, and the death of Betsy Arakawa, wife of the late actor Gene Hackman, from hantavirus in their Santa Fe home in New Mexico (CBS News, April 15, 2025, accessed August 2025). These tragedies have raised awareness about this rare but potentially deadly illness transmitted by rodents. In this article, we provide information on the diseases caused by hantaviruses and what you can do to reduce risk.
Modified recommendations provided by the Centers for Disease Control (CDC)
What are hantaviruses?
Hantaviruses are a group of viruses that cause serious diseases and can be fatal. The viruses primarily infect rodents. People become infected through exposure to the urine, feces or saliva of an infected rodent. Most people get sick after inhaling virus-contaminated bodily fluids from rodents, their waste, or contaminated nesting materials. Rodent bites and scratches can also lead to transfer of the virus, as can consumption of contaminated food (Figure 1).
The hantaviruses that cause hantavirus pulmonary syndrome (HPS) are of the greatest concern to residents. In both Arizona and other contiguous states, the most common hantavirus strain is the Sin Nombre virus which can cause HPS. This virus is spread by deer mice in the genus Peromyscus. The hantavirus strain referred to as Seoul virus can cause hemorrhagic fever with renal syndrome. This is rare in the U.S. and has not been detected in Arizona.
The Centers for Disease Control and Prevention (CDC) report 864 cases of hantavirus infection nationwide between the beginning of surveillance tracking in 1993 and December 2022 (Figure 2, Centers for Disease Control and Prevention. June 26, 2024a, accessed August 2025). During January 2023 through December 2024 more than 60 additional cases have been reported by Health Departments in Arizona, Colorado, New Mexico, Washington, and California.
Most hantavirus infections occur in states west of the Mississippi River. While human cases are considered rare, they can be fatal and approximately 1 in 3 people with HPS who develop respiratory symptoms die from the disease.
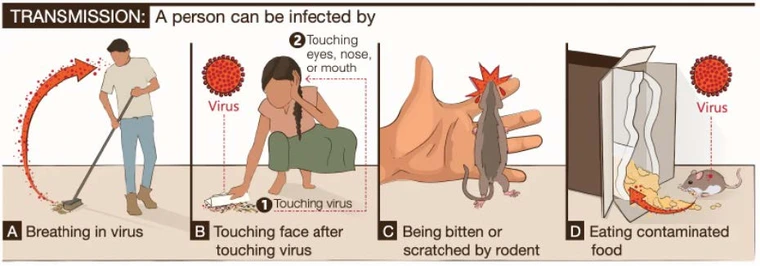
Figure 1. How people become infected by hantavirus.
Excerpted from Centers for Disease Control and Prevention
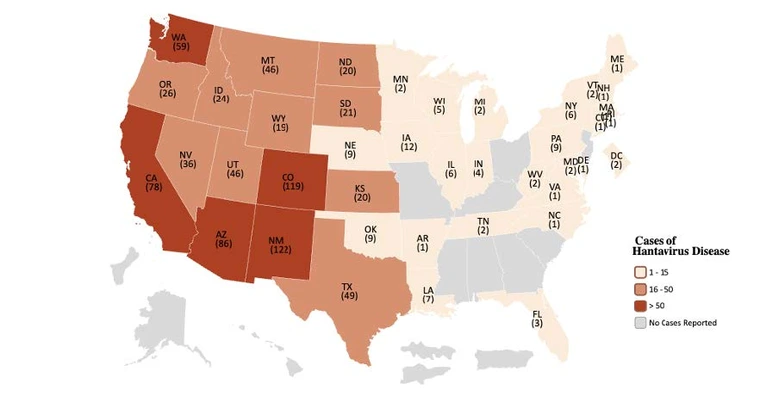
Figure 2. Map of U.S. Cumulative Cases of Hantavirus by State 1993 through 2022 that met the National Notifiable Diseases Surveillance System case definition at the time of reporting, including 31 historical cases that occurred prior to 1993, but were confirmed retrospectively. Five cases have presumed exposure outside the United States.
Centers for Disease Control and Prevention
Where is hantavirus found in Arizona?
While hantavirus is found throughout the Southwestern U.S., it is especially prevalent in the Four Corners region where it was first identified in 1993. In Arizona there were eleven confirmed cases of hantavirus between 2016 to 2022, four of which were fatal. Most of the cases were in northern Arizona, with six in Apache County, three in Coconino County, one in Navajo County, and one in Maricopa County. Arizona experienced a spike in hantavirus cases in 2023 and 2024, with six and eleven confirmed cases, respectively. All but one person developed HPS and unfortunately six people died. Additionally, Pima County recorded the second case ever diagnosed in the county during 2024 (Arizona Department of Health Services (a), last accessed, August 22, 2025).
How is hantavirus spread?
Hantaviruses in the U.S. are not spread from person to person. Hantavirus is typically spread by wild rodents including deer mice (Figure 3), though multiple small mammal species, such as wood rats (Neotoma spp.) and hispid cotton rats (Sigmodon hispidus), can carry and shed virus in their saliva, urine, and droppings (Goodfellow et al. 2025). The deer mouse Peromyscus maniculatus (Figure 4) is most common in prairie, bushy, and woodland habitats (King 1968) throughout the region. The white-footed mouse (Peromyscus leucopus) (Figure 5) is most abundant under 6,500-foot elevation, and the western deer mouse (Peromyscus sonoriensis) (Figure 6) is considered to be a primary reservoir for the Sin Nombre virus (Goodfellow et al. 2025), in most areas, although more prevalent in the western and central areas of Arizona.
A person may be exposed to hantavirus by breathing contaminated dust after disturbing or cleaning rodent droppings or nesting materials. Living or working in rodentinfested settings increases the chance of exposure. A person can be exposed when entering unused buildings or coming into contact with rodent burrows outdoors. Rarely, individuals can be infected by consuming food contaminated with rodent urine or droppings or by being bitten or scratched by infected rodents (Arizona Department of Health Services (b), last accessed, August 22, 2025). Dogs and cats do not typically develop symptoms of illness when infected with Sin Nombre virus and cannot spread the virus directly to other animals or humans. However, they can put people at risk indirectly by bringing infected rodents into homes or buildings where exposure to infected rodent excretions may occur. Canines can be affected by other hantaviruses and develop illness.
Hantavirus pulmonary syndrome signs and symptoms
Hantavirus pulmonary syndrome is a severe and potentially fatal illness caused by some hantaviruses found in the Western Hemisphere. The viruses affect lung function, impacting breathing.
Early symptoms (usually 1-8 weeks after exposure) include fatigue, fever, muscle aches, headaches, dizziness, chills and abdominal problems like nausea, vomiting, diarrhea or abdominal pain.
Later symptoms (usually 4-10 days after initial phase of illness) include coughing and shortness of breath or tightness in the chest as the lungs fill with fluid.
Treatment and recovery
If you believe you may be experiencing symptoms of hantavirus, or been exposed to the virus, seek medical care.
There are currently no U.S. Food and Drug Administrationapproved hantavirus vaccines available in the United States. There are no specific antiviral medications for infections. Treatment focuses on supportive care to manage symptoms and maintain organ function until the body can fight off the virus. This often involves intensive care in a hospital setting, which may be crucial for recovery.
Early symptoms are often non-specific and mimic other viral illnesses, making diagnosis challenging. HPS diagnosis relies on a combination of clinical evaluation, history of potential rodent exposure, and laboratory tests. Testing for hantavirus antibodies in the blood is the primary diagnostic tool. The CDC uses an enzyme-linked immunosorbent assay to detect IgM antibodies and diagnose acute infections of hantaviruses.
Prevent hantavirus infection
The best way to prevent hantavirus infection is to avoid exposure to rodents, their urine and feces. You can concurrently seal up to prevent rodents from entering buildings, clean up to remove contaminated waste, and “trap up” to reduce rodents in buildings (Centers for Disease Control and Prevention, 2021, accessed August 2025).
TRAP UP: Trap rodents to reduce populations in or around buildings
- Deer mice (Peromyscus spp.) and house mice (Mus musculus) have distinct differences in appearance, habitat, diet and behavior. See more information below.
- Although house mice are unlikely hantavirus reservoir hosts, you should avoid harboring them in your home or buildings for other health related reasons.
- Containerized traps can be used to catch and remove rodents that are found in or around buildings. Snap traps are among the most common traps used for rodent control. Avoid using glue traps or cage (live) traps because these traps can scare rodents causing them to void urine and defecate (urinate and poop), which can increase exposure risks.
- Selecting the correct traps is important and you want to consider criteria such as trap size, expanded trigger, easiness to set, and what lure to use. Any type of trap efficacy can vary depending on factors such as what the local rodents are feeding on, trap placement, and environmental conditions. Many types and makes of traps can be used to catch deer mice. For example, the Goodnature ® CO2 A24 guillotine device has demonstrated effectiveness against Peromyscus mice in field situations (Gilliland 2020), and carcass removed by scavenging animals can be an additional benefit of these traps.
- Baits can be toxic (rodenticides) or non-toxic (bait that tells the applicator if the rodents are in the area). Many rodenticides can only be used by licensed pest management professionals, but some are available to the public. Baits must be applied according to the label. Inside or around homes toxic baits should only be used in tamper-proof bait stations that prevent children, pets or other non-target animals from accessing the rodent bait. Baiting works best when used in conjunction with other methods like trapping, sealing entry points and eliminating food sources. Information obtained from building inspections can be used to place bait in active rodent runways to improve control, and eliminating food sources encourages rodents to feed on bait.
Deer Mouse | House Mouse |
|---|---|
| Brown or tan with clearly demarcated white bellies, legs and feet. | Light brown or gray with solid color coats. No clear demarcation between upper and lower body colors. |
| Tend to store scavenged food near nests. | Consume food as they find it. |
| Usually 3-4 inches, some can reach up to 7 inches. | Usually 2-3 inches, never longer than 5 inches, including the tail. |
| Deer mice are carriers of the hantavirus. | Unlikely hantavirus reservoirs but can bring pests like lice and fleas into homes. |
| Found in rural and wooded areas. May invade homes and buildings. | Commonly found in homes and buildings |
SEAL UP: Seal up to prevent rodents from entering buildings
- Conduct regular inspection and monitoring to determine whether and why rodents are present, where they nest and how they access the building. Fill any gaps or cracks that allow a pencil or pen to fit through as these are large enough for a deer mouse to use as an entry point. Look for signs of rodent infestation, such as live or dead rodents, droppings, foot and tail tracks in dust, urine stains, dark rub marks, gnawing damage and burrows. Also look for conducive conditions, such as food, moisture and access to shelter, which will attract them.
- Seal holes and gaps in external walls, doors, and windows of homes or garages. Use concrete, rodent fabric (e.g., Xcluder ® rodent fabric or STUF-FIT copper mesh), or steel wool to block potential entryways. Store food securely. Keep food in airtight containers and clean up crumbs and spills promptly. Use door sweeps specifically designed with rodent exclusion in mind in high-risk areas.
- Remove food and water sources to make the place less attractive. De-cluttering is essential for successful rodent management.
- Reduce rodent attractants around the home, work, and recreational areas. Remove debris, branches, firewood, fruit and other food sources. Remove items near your home that could provide nesting sites, such as piles of wood or stones. Reduce clutter around the yard and property. Move trash bins away from building doorways whenever possible. Trim tree branches and shrubs near your home and clear away leaves and brush piles that build up against buildings.
CLEAN UP: Clean up safely
Ventilate the space: Open all doors and windows and leave the building to air out for 30 minutes before entering to undertake tasks.
Use protective gear: Wear a respirator with a High-Efficiency Particulate Air (HEPA) filter, unvented protective goggles, and impermeable latex or rubber gloves. For heavy infestation CDC recommends using a half mask air-purifying (or negative-pressure) respirator with a high efficiency particulate air (HEPA) filter. A powered air-purifying respirator (PAPR) with HEPA filters can also be used.
Avoid sweeping or vacuuming: Do not sweep or vacuum contaminated areas because this can stir up harmful particles, make them airborne, and inhaled by people.
Disinfect thoroughly: Spray dead rodents, urine, droppings, nesting materials and affected areas with an EPA-registered disinfectant before cleaning. Follow the directions of use for the specific disinfectant used. Or use a 10% bleach solution (made by mixing 1 part bleach with 9 parts water) and spray down areas where rodent/mouse droppings or nests are found and allow the solution to soak for at least 15 minutes to kill any hantavirus. Use wet disposable towels to wipe up the disinfected droppings and nesting materials.
Clean equipment: Place materials and used towels into a plastic bag and tie the bag. Place inside a second bag and place in an external dumpster. Mop or clean the area. After cleaning, disinfect protective gear with an EPA-registered disinfectant, then again with soap and water, and allow it to air dry before reuse. Dispose of gloves in the trash. Then wash hands with soap and water.
Handle traps and carcasses safely: Spray dead mice with an EPA-registered disinfectant before disposal. Avoid handling carcasses directly and dispose of them in a sealed plastic bag in an outdoor trash receptacle while wearing protective gear.
Precautions when handling dead rodents
- Wear disposable rubber or plastic gloves.
- Spray the dead rodent and any trap with disinfectant until wet.
- With a hand inside a disposable plastic bag, pick up the rodent and the trap if one is associated, and invert the bag over the rodent and seal or tie the bag with the rodent and trap inside.
- Place the bag in a second plastic bag and discard in an external dumpster outside of the home.
- Spray the area where the trap or the dead rodent was lying with 10% bleach solution (made by mixing 1 part bleach with 9 parts water) or a disinfectant. Follow the directions of use for the specific disinfectant used.
- Wash gloved hands with soap and water or a disinfectant before removing gloves. Dispose of gloves in the trash.
- Wash hands with soap and water after removing gloves.
In the table below (Table 3), we summarize some important guidance. Visit the CDC website for precaution recommendations when cleaning to reduce risk to hantavirus exposure.
Summary
- Hantavirus is transmitted when humans come into contact with infected rodents and their feces, urine, and saliva.
- You can get infected by breathing dust that has been contaminated with hantavirus, being bitten or scratched by infected rodents, or on rare occasions consuming contaminated food.
- Immediate supportive care is essential to save lives. ▪ Approximately 1 in 3 people with hantavirus pulmonary syndrome die, so do not delay seeking medical care.
- Hantavirus infection is preventable by taking precautions when cleaning and entering spaces where rodents have been recently occupying. Hantaviruses do not persist for long periods of time in warmer temperatures, but it is often impossible to know when an infected rodent was last in a building.
- DO NOT sweep or vacuum rodent urine, droppings, or nesting materials. It can stir up the virus in airborne particles that may be inhaled.
- Take precautions when handling a dead rodent. Safely dispose of dead rodents. Clean up and disinfect areas contaminated with rodent urine and droppings.
Does Work | Does Not Work |
|---|---|
| Wear disposable rubber or plastic gloves. | Fabric gloves since gloves should maintain a barrier between people and rodent urine/feces and be properly disposed of after use. Fabric gloves do not provide an effective barrier against rodent urine and feces. The porous material of fabric allows harmful pathogens to pass through, increasing risk of exposure. |
| Spray urine and droppings with 10% bleach solution (mixing 1 part bleach with 9 parts water) or an EPA-registered disinfectant. | Soap water or other natural cleaning solutions as this does not disinfectant (destroy hantavirus). |
| Wipe up the disinfected droppings and nesting materials with paper towels. | Sweep or vacuum contaminated areas as this can stir up harmful particles and aerosolize them, increasing risk of exposure. |
| Containerized snap or guillotine traps. | Glue traps or cage (live) traps as after being trapped, mice tend to poop and urinate, increasing risk of exposure. |
Acknowledgment
This material is based upon work that is supported by the National Institute of Food and Agriculture, U.S. Department of Agriculture, under award 2024-70006-43563. Any products, services, recommendations or organizations mentioned, shown, or indirectly implied in this publication do not imply endorsement by the USDA, Arizona Department of Health Services, or University of Arizona.
References
Arizona Department of Health Services (a). Hantavirus - Information & Data. https://www.azdhs.gov/preparedness/epidemiology-disease-control/vectorb…. Last accessed, August 22, 2025.
Arizona Department of Health Services (b). Hantavirus Home. https://www.azdhs.gov/preparedness/epidemiologydisease-control/vector-b…. Last accessed, August 22, 2025.
CBS News. April 15, 2025. https://www.cbsnews.com/news/betsy-arakawa-researched-hantavirus-pulmon…. Last accessed, August 22, 2025
Centers for Disease Control and Prevention. 2021. You Can Prevent Hantavirus. https://www.cdc.gov/hantavirus/media/pdfs/2025/01/HantavirusBrochure-50…. Last accessed, August 22, 2025.
Centers for Disease Control and Prevention. June 26, 2024a. Reported Cases of Hantavirus Disease. https://www.cdc.gov/hantavirus/data-research/cases/index.html. Last accessed, August 22, 2025.
Centers for Disease Control and Prevention. May 13, 2024b. About Hantavirus. https://www.cdc.gov/hantavirus/about/index.html. Last accessed, August 22, 2025.
Centers for Disease Control and Prevention. April 8, 2024c. How to Clean Up After Rodents. https://www.cdc.gov/healthy-pets/rodent-control/clean-up.html. Last accessed, August 22, 2025.
Gilliland, K. L. 2020. Use of A24 self-resetting traps for California ground squirrel (Otospermophilus beecheyi) control. In: Woods DM (ed) (2020) Proceedings of the 29th Vertebrate Pest Conference, University of California, Davis, USA, pp 1–7.
Goodfellow, S.M., Nofchissey, R.A., Ye, C., Banther-McConnell, J.K., Suriyamongkol, T., Cook, J.A., Dunnum, J.L., Mali, I. and Bradfute, S.B. Jan 2025. A human pathogenic hantavirus circulates and is shed in taxonomically diverse rodent reservoirs. PLOS Pathogens. https://doi.org/10.1371/journal.ppat.1012849.
King, J. A. 1968. Biology of Peromyscus (Rodentia). First Edition. The American Society of Mammalogists, Stillwater, Oklahoma.






